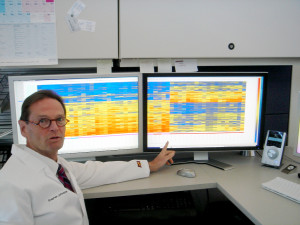
Stephen Albert Johnston pictured in front of computer monitors displaying portraits of immune activity known as immunosignatures. Johnston directs Biodesign’s Center for Innovations in Medicine.
Photo by: The Biodesign Institute at Arizona State University
Despite impressive medical strides, cancer remains a leading killer and overwhelming burden to health care systems, causing well over a half million fatalities per year, with a projected cost of $174 billion by 2020, according to the National Cancer Institute. Reducing the human and economic toll will require diagnosis and intervention at early stages of illness, when the best prognosis for a cure exists.
In research appearing in the July 14 issue of the journal Proceedings of the National Academy of Science, Stafford and his team describe an innovative technique for early disease detection, which they call immunosignaturing.
“For years we’ve seen remarkable results from immunosignatures, but introducing the technology to the scientific community has required a lot of patience,” Stafford says. Stafford is a researcher in Biodesign’s Center for Innovations in Medicine, which is co-directed by Stephen Albert Johnston, who is also one of the new study’s co-authors and a professor in ASU’s School of Life Sciences.
To date, only a handful of cancer biomarkers have received FDA approval for clinical use, and even approved biomarkers are sometimes of limited utility. The problems are numerous. The body’s immune response to cancer is complex, heterogeneous and differs from patient to patient, as well as depending on cancer type and stage.
Individual biomarkers often lack the sensitivity and resolution for positive diagnosis and diagnostic molecules, including RNA, DNA and proteins or peptides, are often present in vanishingly slight amounts after diluting in the bloodstream, making accurate detection especially challenging. Vast research efforts notwithstanding, efforts to establish better pre-symptomatic beacons of disease have been disappointing.
Immunosignatures take a different approach. Rather than using a reductionist biomarker paradigm, it relies on a multiplexed system in which the entire population of antibodies circulating in blood at a given time is profiled.
The technique relies on a microarray consisting of thousands of random sequence peptides, imprinted on a glass slide. (The peptides used are 20-unit amino acid chains, randomly composed.)
When a tiny droplet of blood (less than a microliter is needed) is spread across the microarray, antibodies in the blood selectively bind with individual peptides, forming a portrait of immune activity – an immunosignature.
Because the peptide sequences are random and not related to any naturally occurring disease antigens, the authors refer to immunosignatures as “disease agnostic,” which means that a single platform is potentially applicable to multiple disease types. This is a substantial improvement over highly specific bioassays that can only test for a single biomarker antibody, often with substantial misidentification or inadequate sensitivity.
The current study puts immunosignatures to the test, evaluating the technique’s ability to identify multiple disease types. The team first “trained” the system to calibrate results and establish reference immunosignatures using 20 samples each from five cancer patient cohorts, along with 20 non-cancer patients. Once reference immunosignatures were established, the technique was tested in a blind evaluation of 120 independent samples covering the same diseases. The results demonstrate 95 percent accuracy.
To further assess the diagnostic power of immunosignaturing, over 1,500 historical samples comprising 14 different diseases, including 12 cancers, were tested. In this case, 75 percent of the samples were used in the training phase, and the remaining 25 percent were subjected to blind test.
Remarkably, an average diagnostic accuracy of over 98 percent was achieved, demonstrating the suitability of immunosignaturing for the simultaneous classification of multiple diseases.
Specifically, in one experimental trial, researchers were able to detect and distinguish a complex, heterogeneous disease – stage IV breast cancer, relative to four other cancers and healthy controls. In the second trial, 14 separate diseases were distinguished from one another, as well as from healthy controls, through immunosignatures. Among the cancers tested were three different stages of breast cancer, four different brain cancers, two pancreatic diseases, ovarian cancer and two different blood cancers.
The study emphasizes the fact that incidence of cancer constitutes an unprecedented global challenge to health care infrastructure, particularly in the face of aging populations. Early detection and treatment of cancer must be given highest priority in order to adequately address projected increases in cancer cases.
Immunoisignatures provide an attractive means of capturing disease complexity, offering a marked improvement in detection over traditional methods in which one-to-one molecular recognition events are measured, and only one or a small number of analytes can be evaluated.
In addition to the problem of dilution of measurable analytes in conventional tests, the authors stress the considerable heterogeneity of cancer, which results in complexity at the molecular level that tends to evade characterization when only a few target analytes are evaluated.
The microarray chip used for the current study contains 10,000 imprinted peptides, of random sequence, which serve the role of artificial disease antigens used to poll the antibodies present in blood. The fact that the random sequence peptides are structurally unrelated to natural antigens allows the array to perform as a sort of all-purpose diagnostic, capable of producing an antibody profile or immunosignature, regardless of the underlying disease in question.
When a particular immunosignature is recorded, some of the antibody activity observed pertains to binding signals present in most individuals; some are unique to particular individuals. In the case of underlying disease however, a subset of binding signals will be the result of disease-related antigens common to most individuals with the same disease, making the results highly reproducible.
The presence of 10,000 peptides on each microarray chip allows for enhanced sensitivity, owing to the large number of different possible signals elicited. The technology is also highly flexible in terms of handling and processing. A dried sample of blood, collected on filter paper and mailed to a study facility can be used to generate an immunosignature, permitting frequent health monitoring at a low cost.
Further, a significant improvement in immunosignaturing sensitivity and accuracy can be achieved through new chip technology. The group is currently developing a peptide imprinted with greater than 100,000 peptides.
