Despite enormous progress, breast cancer remains elusive, perplexing and, often, deadly. The disease can emerge due to a complex interplay of factors, including lifestyle, environment, aging and genetic predisposition.
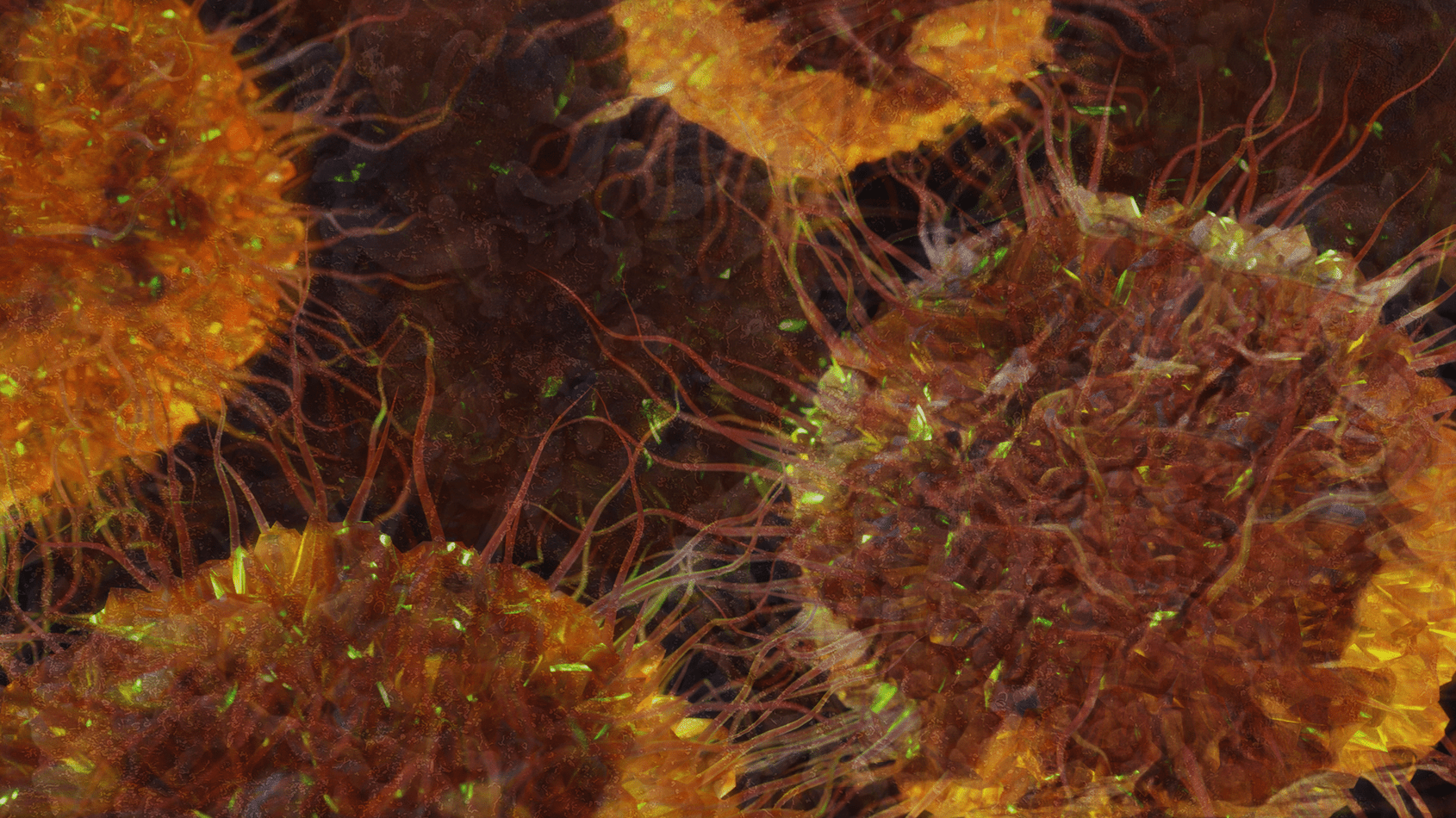
Illustration of tumor cells. A new study examines mutations in the cancer suppressor gene TP53, which can lead to an aggressive, treatment-resistant disease known as triple-negative breast cancer. Graphic by Jason Drees
In a groundbreaking new study — 10 years in the making — co-corresponding authors Joshua LaBaer and Jin Park, along with their Arizona State University colleagues, found that certain mutations in a gene known as TP53 can dramatically alter the aggressiveness of cancer-related characteristics.
Intriguingly, this gene has been recognized as a cancer suppressor since the 1970s, but TP53 can also advance the disease when the gene becomes mutated, producing an altered form of the protein p53. This often occurs in so-called “triple-negative breast cancer,” a virulent version of the illness that often carries a bleak prognosis.
The researchers explored 10 clinically common p53 mutations. After inserting these mutations into cell lines, the researchers found a range of cell behaviors reflecting varying degrees of cancer aggressiveness. The effects of the mutations were analyzed in terms of cell survival, resistance to cell death (apoptosis), cell invasion and other cancer-related characteristics.
A cell line is a group of cells that are continually propagated or cultured outside the organism, usually in a lab dish or flask, allowing for the indefinite study of the cells. They are often derived from a single cell and thus represent a population of cells that are genetically identical.
The cells we used for the study were breast cells that engage in natural behavior like the formation of glands and ducts that mimic behavior in normal breast development.
Four specific mutants were identified as the most aggressive, correlating with worse survival rates in basal-like breast cancer patients. The findings also indicate that in some cases, a mutated form of p53 can cause a gain-of function in altered cells, enhancing rather than suppressing the transition to resistant forms of cancer.
The researchers compared their laboratory results with databases of breast cancer cases, implicating a specific biological pathway — known as Hippo/YAP/TAZ. This pathway is particularly active when aggressive p53 mutants are present and appears to play a crucial role in cancer aggressiveness.
The study provides valuable insights into how specific p53 mutations can lead to various outcomes in triple-negative breast cancer, potentially informing future therapeutic strategies.
“This form of breast cancer is especially common in younger women and women of color,” LaBaer says. “It is not only more aggressive, but it doesn’t respond to many of our latest treatment strategies. That is why it was so important to find pathways that will guide us to new therapies.”
LaBaer is the executive director of the Biodesign Institute at ASU and director of the Biodesign Virginia G. Piper Center for Personalized Diagnostics, where Park is an associate research professor.
The research appears in the current issue of the journal npj Breast Cancer.
Breast cancer originates from abnormal cells in the breast, which can multiply uncontrollably and become life-threatening. In 2020 alone, this cancer touched the lives of 2.3 million women, claiming 685,000 of them. About half of those affected had no particular risk factors besides being female and of a certain age. Men also face this diagnosis, though rarely, making up just 0.5 to 1% of cases.
Gender and age top the list of risk factors, though lifestyle choices, including diet and alcohol consumption, family medical history and specific mutations in genes like BRCA1 and BRCA2 can tilt the scales.
Once diagnosed, treatment is tailored to the individual, considering factors like the type of cancer and how far it has spread. Treatments may include surgery, radiation therapy and chemotherapy. Hormone therapies may be applied for hormone-sensitive cancer types, while chemotherapy is often the standard of care for hormone-insensitive cancers.
Triple threat
While genetic mutations in general can increase breast cancer risk, specific mutations like BRCA1 and BRCA2 lead to a much higher lifetime risk. Knowing your specific mutation can help determine the best prevention and screening actions.
Triple-negative breast cancer is a type of breast cancer that lacks three common protein receptors used by physicians to target the disease: the estrogen receptor, progesterone receptor and HER2. Because these receptors are not present in the triple-negative cancers, common treatment approaches such as hormone therapy don’t work well.
Treatment for triple-negative breast cancer typically involves surgery (lumpectomy or mastectomy) followed by chemotherapy. Radiation therapy may also be used after a lumpectomy. The goal is to remove the tumor and use chemotherapy to kill any remaining cancer cells that have spread.
Since triple-negative breast cancer can run in families, genetic counseling may be advised for those at risk. By understanding the characteristics and typical treatment approach for this type of breast cancer, patients can work with their medical team to determine the best options.
Role as a genetic sentry
The TP53 gene has long been recognized by biologists as the “guardian of the genome” for its remarkable ability to suppress cancer in species across the tree of life. It has recently been shown that certain large species, including elephants, seem to benefit from multiple copies of the p53 protein, which may be crucial for their longevity and exceptionally low rates of cancer.
The p53 protein accomplishes its cancer-crushing activities in a variety of ways. For example, by repairing damaged DNA, it prevents the accumulation of mutations that could lead to cancer. Also, the protein can act to pause the cell cycle, giving the cell additional time to repair DNA damage before it divides.
Where irreparable damage to the DNA has occurred, p53 can induce programmed cell death to prevent aberrant cells from proliferating. p53 can also suppress the formation of new blood vessels (angiogenesis) that tumors need for their growth and progression. Additionally, the protein plays a role in modulating immune responses, helping the body eliminate cancerous cells through the immune system.
Different mutations cause different effects
The study explores 10 of the most common missense mutations and the cellular behavior resulting from mutated p53 proteins. A missense mutant is a type of genetic mutation that results in a single amino acid change in the encoded protein. The resulting protein is the same length as its normal counterpart but has slightly altered structure and chemistry due to the replaced amino acid. This can impair or alter the protein’s function and lead to disease.
For example, a common missense mutation in the p53 tumor suppressor gene substitutes arginine for proline at position 53. This mutation impairs p53’s cancer-preventing function, promoting tumor growth. Roughly 80% of triple-negative breast cancer cases involve p53 mutations.
In highly aggressive cancers, missense mutations are the most common. This is unusual for tumor suppressors, which are often inactivated by more straightforward “loss-of-function” mutations, such as nonsense mutations or frameshift mutations that clearly incapacitate the protein. In contrast, missense p53 mutations can not only cause the loss of tumor suppressor activity but may be related to acquiring new activities that encourage tumor growth, making these mutations crucial in cancer research and treatment strategies.
Four specific p53 mutants were identified as the most aggressive, correlating with worse survival rates in basal-like breast cancer patients. The study also explores biochemical pathways that may help to account for the stark differences in cell behavior caused by the various mutations.
Comparing their findings with existing datasets on breast cancer cell lines and tumors, the researchers concluded that one of these pathways — known as Hippo/YAP/TAZ — plays a key role in driving cancer invasiveness, especially in the presence of aggressive p53 mutants.
“By systematically testing the 10 most clinically important p53 mutants by an integrative approach of merging cancer biology, genomics, and bioinformatics, we unveiled drug-targetable pathways for more effective and personalized treatment of triple-negative cancers with specific p53 mutations,” Park says.
Deepening the understanding p53’s role in cancer suppression and the specific ways mutations can derail this cancer-fighting system opens the door to new strategies to address breast and other cancers, particularly resistant variants.
Discoveries Tempe campus Biodesign Institute Biodesign Virginia G. Piper Center for Personalized Diagnostics School of Molecular Sciences Bioscience Health care Research Faculty TRIF
Byline:
Richard Harth
Science writer, Biodesign Institute at ASU
480-727-0378 richard.harth@asu.edu
October 4, 2023
