TGen, Phoenix Children’s Hospital and Barrow Neurological Institute lead study of traumatic brain injuries following stroke
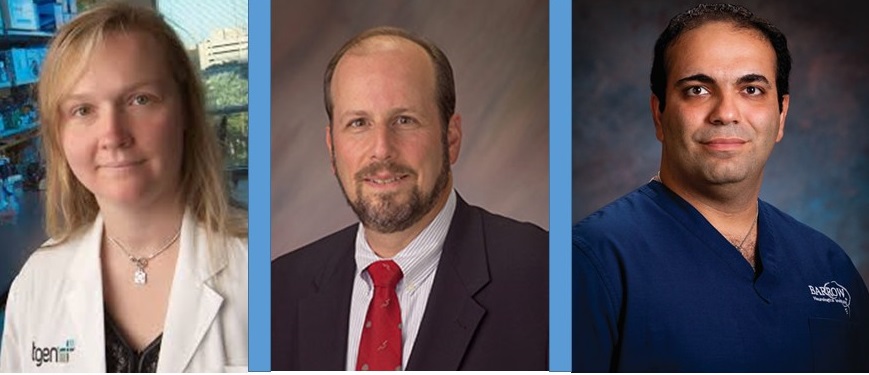
Kendall Van Keuren-Jensen, PhD of TGen’s Neurogenomics Division; P. David Adelson, MD, FACS, FAAP at the Barrow at Phoenix Children’s Hospital; and Yashar Kalani, MD, PhD of Barrow Neurological Institute,
PHOENIX, Ariz. — Sept. 9, 2015 — Developing better treatments and an improved understanding of the biology behind brain injury from hemorrhagic strokes is the main goal of a three-year $2.8 million grant to the Translational Genomics Research Institute (TGen), Phoenix Children’s Hospital, and Barrow Neurological Institute. Announced today, the funding comes from the National Institutes of Health’s National Center for Advancing Translational Sciences (NCATS) under its Extracellular RNA (ExRNA) Communication program.
Hemorrhagic strokes occur when a blood vessel bursts in the brain and blood accumulates and causes injury to the surrounding brain tissue, often leading to rare but devastating types of traumatic brain injuries (TBIs).
In this study, researchers seek to identify exRNAs suitable as biomarkers to indicate the severity of hemorrhagic stroke and risk of subsequent injury. Biomarkers are indicator molecules — such as proteins, DNA, or RNA — measurable in blood, body fluids or tissue samples that can aid in the diagnosis or severity of a particular disease or the effects of a given treatment.
“Because exRNAs are released from all tissues in the body, including the brain, they make an ideal candidate as a biomarker to help doctors in the evaluation and treatment of patients with brain injury,” said Kendall Van Keuren-Jensen, Ph.D., an Associate Professor in TGen’s Neurogenomics Division, and one of the study’s principal investigators. “Ultimately, this research could lead to the development of new treatments and improved outcomes in hemorrhagic stroke patients.”
In adults, this type of stroke occurs annually in 10-15 people per 100,000, and the risk of these strokes increases with age.
“Scientists still do not fully understand what goes wrong in the brain during and after stroke, and this study will be an important step toward better defining the biological underpinnings of not only stroke, but brain injury in general” said Yashar Kalani, M.D. and Ph.D., a chief resident in Neurological Surgery, assistant professor at Barrow Neurological Institute, and a principal investigator on the study.
The project will focus on two subtypes of hemorrhagic events: aneurysmal subarachnoid hemorrhage; and pediatric intraventricular hemorrhage, which is a significant complication of premature infants.
“We are especially concerned about how these types of brain injury affect children and their ability to recover from such trauma but also develop new and innovative approaches for treating TBI,” said P. David Adelson, M.D., Director of BNI at PCH, Chief Pediatric Neurosurgeon at PCH, and an internationally recognized expert in the area of pediatric traumatic brain injury. He also is one of the study’s principal investigators.
An extracellular RNA (exRNA) biomarker to predict onset and severity of brain hemorrhage would have an immediate effect on improving patient outcomes, as well as to reduce significant costs to patients and caregivers.
Until recently, scientists believed RNA worked mostly inside the cell that produced it. Some types of RNA help translate genes into proteins that are necessary for organisms to function. Other types of RNA control which proteins and how much of those proteins the cells make.
Now, investigators have shown that cells can release RNA — in the form of exRNA — to travel through body fluids and affect other cells. ExRNA can act as a signaling molecule, communicating with other cells and carrying information from cell to cell throughout the body.
A better understanding of basic exRNA biology could open doors to improving the diagnosis, prognosis and treatment of diseases and conditions such as cancer, bone marrow disorders, heart disease, Alzheimer’s disease and multiple sclerosis.
# # #
About TGen
Translational Genomics Research Institute (TGen) is a Phoenix, Arizona-based non-profit organization dedicated to conducting groundbreaking research with life changing results. TGen is focused on helping patients with neurological disorders, cancer, and diabetes, through cutting edge translational research (the process of rapidly moving research towards patient benefit). TGen physicians and scientists work to unravel the genetic components of both common and rare complex diseases in adults and children. Working with collaborators in the scientific and medical communities literally worldwide, TGen makes a substantial contribution to help our patients through efficiency and effectiveness of the translational process. For more information, visit: www.tgen.org. Follow TGen on Facebook, LinkedIn and Twitter @TGen.
Press Contact:
Steve Yozwiak
TGen Senior Science Writer
602-343-8704
syozwiak@tgen.org
